In office transperineal prostate biopsy with local anaesthesia
Prostate biopsy is the necessary step for making the diagnosis of prostate cancer once this is suspected based on abnormal MRI, prostate specific antigen (PSA) or abnormal rectal examination. The biopsy provides multiple small samples of prostate tissue for pathological examination. The traditional method of transrectal ultrasound biopsy (TRUS), due to low detection rate and higher infection rate is no longer recommended. In Australia, the transperineal prostate biopsy has become the procedure of choice for sampling the prostate and is routinely carried out in the hospital under general anaesthesia. Recent experience from UK and USA has demonstrated that this method of biopsy can be safely carried out in the office setting and under local anaesthesia without the need for hospital admission and general anaesthesia. Doctor Zargar has adopted and refined this method of biopsy over the past 18 months and we are the only practice in Victoria that offers transperineal prostate biopsy under local anaesthesia in the office setting.
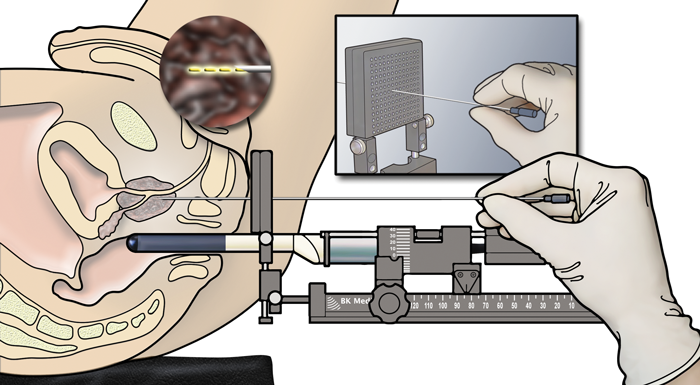
On the day of the procedure, patient arrives at the office. The patient sits on our examination couch and the couch is flattened and the legs are slightly elevated. The scrotum is pulled up and secured. The rectal exam is carried out and the perineum is cleaned with antiseptic solution. The ultrasound probe is gently placed within the rectum and prostate is visualised.
Small volume of local anaesthesia is placed under the skin followed by injection around the prostate to numb the area of biopsy. After few minutes interval the biopsy is carried out. Depending on the findings on MRI 8-24 prostate samples are obtained. Typically 1-4 puncture sites at the perineal skin are made to access the prostate.
The initial injection of local anaesthesia can be somewhat painful but it is well tolerated by the patients. Once the local anaesthesia is achieved. the procedure can be carried out without any significant discomfort. Patient can still feel the movements of the instruments but would not experience any pain. The procedure takes about 30 minutes. After the procedure pain is minimal and is well controlled with oral pain relief.
The risk of infection and bleeding in the urine after the procedure is very low. Observing blood in the semen up to 6 weeks after the procedure is extremely common. Risk of difficulty with urination or need for a urinary caterer is around 1%. Patient can return to normal activities in 1-2 days. Sexual activities can resume at the same time.
This short video prepared at James Buchanan Brady Urological Institute is an excellent summary of different methods and the rationale behind our current approach.