prostate
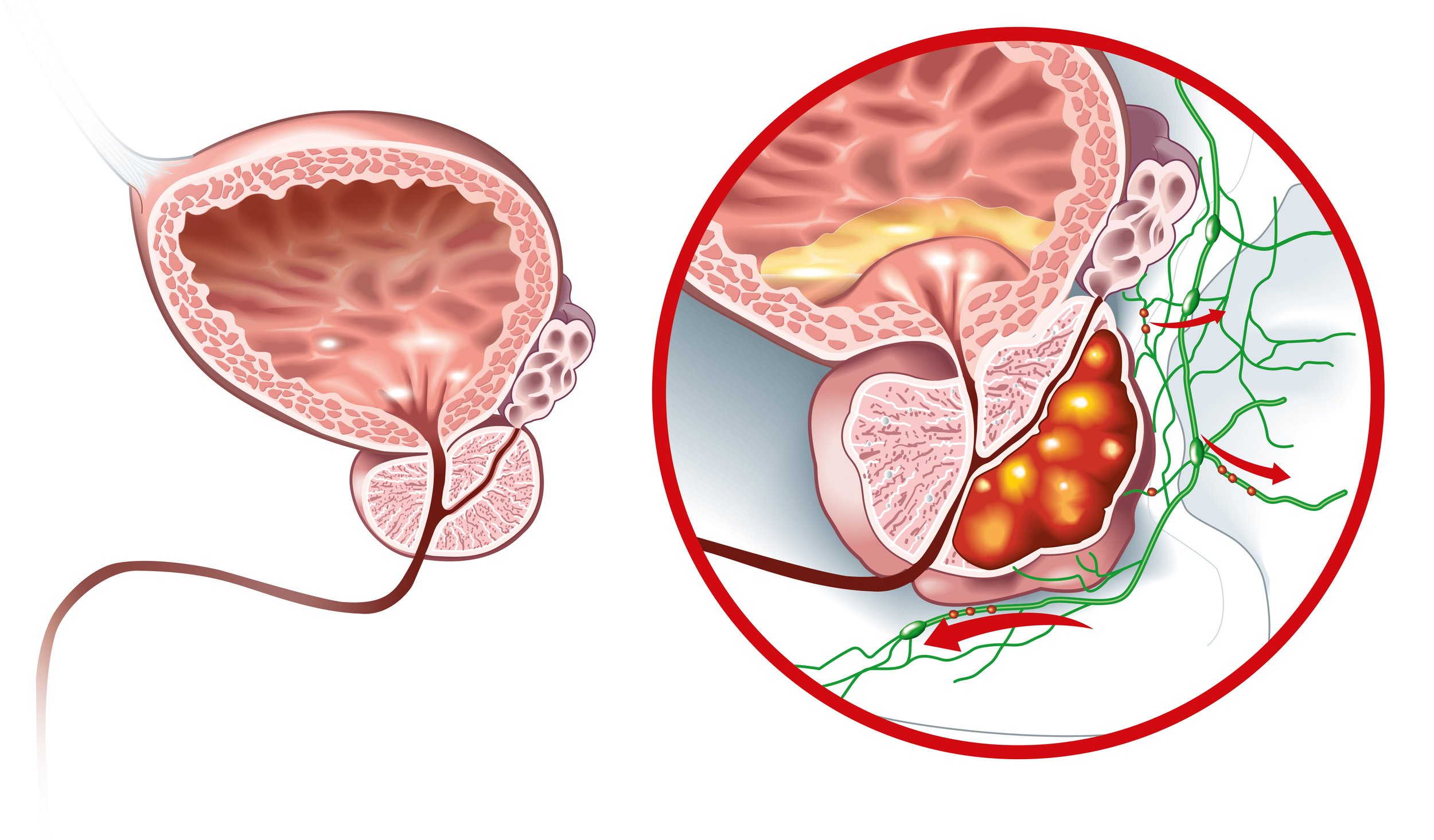
prostate cancer
Prostate cancer is the most commonly diagnosed cancer in Australian men. It often develops silently, and most men are asymptomatic at the time of diagnosis. Early detection through PSA testing and appropriate follow-up imaging has dramatically improved outcomes.
Risk increases with age, family history, and higher PSA levels at a younger age. Men in the highest 10% of PSA levels between age 45–55 contribute to almost half of prostate cancer–related mortality before age 70–75.
prostate cancer
About one in six Australian men will develop prostate cancer in their lifetime. Prostate cancer typically progresses silently in its early stages, showing no noticeable signs or symptoms. Manifestations may become apparent as the cancer advances and extends to other areas of the body. Advanced stages of prostate cancer may present symptoms such as difficulty in voiding, a weakened or interrupted urine stream, frequent night-time urination, blood in the semen, erectile dysfunction, or bony pain.
The risk of prostate cancer rises significantly with age, with a majority of diagnoses occurring after the age of 65. Individuals with a family history of prostate cancer face an elevated risk, particularly if a close relative, such as a father or brother, has had the disease, doubling the likelihood of prostate cancer development. Notably, men with elevated prostate-specific antigen (PSA) levels at a younger age are at an increased risk of both developing and succumbing to prostate cancer. Those in the highest 10% of PSA concentrations between the ages of 45 and 55 contribute to approximately half of prostate cancer-related deaths before the age of 70-75. Regular screenings and awareness of risk factors remain critical for timely detection and intervention in prostate cancer cases. A/Prof Homi Zargar provides expert prostate cancer care for men in Melbourne and Victoria with personalised diagnosis and treatment plannin
Prostate cancer
The majority of men with prostate cancers at the time of diagnosis are asymptomatic.
the symptoms
Early Stages: Prostate cancer may be asymptomatic in its initial stages, showing no noticeable signs.
Advanced Stages: Symptoms may manifest as the cancer grows and spreads to other parts of the body.
Voiding Issues: Advanced prostate cancer can lead to trouble voiding, characterized by difficulties in urination.
Altered Urine Stream: A weakened or interrupted urine stream may be experienced in later stages.
Nocturia: Increased frequency of urination, particularly at night, may occur as the cancer progresses.
Haematuria: Blood in the semen is a potential symptom, signaling advanced prostate cancer.
Erectile Dysfunction: In later stages, prostate cancer may contribute to erectile dysfunction.
Bony Pain: Advanced prostate cancer may cause pain in the bones, indicating its spread to distant areas.
Individual Variations: Symptoms can vary widely, and their severity depends on the stage and extent of cancer involvement. Regular health check-ups and awareness of risk factors contribute to early detection and intervention.
The majority of prostate cancer in Australia in picked up with PSA testing
What happens after referral
After receiving your referral, our practice nurse will triage your case, and you'll be promptly contacted for a brief overview of your condition. Preceding your visit, several diagnostic tests, urine analysis, PSA test, and bladder/prostate ultrasound are arranged to enhance the evaluation. At your appointment, A/Prof Homi Zargar will engage with you, conduct a thorough assessment, and review the gathered information. If you have an established diagnosis, all your details, including MRI, PET scan, and biopsy results, will be collated prior to your initial assessment.
For a simpler patient-friendly overview of prostate cancer, you can visit the Urology Institute information page here.
Diagnosis of prostate cancer
Modern imaging techniques including MRI scan and PET scan are very helpful tools in the assessment of prostate cancer,
The diagnosis of prostate cancer involves a comprehensive process, often initiated by routine screenings or in response to symptoms. Two primary diagnostic tools are commonly utilized: the PSA (prostate-specific antigen) blood test and a digital rectal exam (DRE). Elevated PSA levels or abnormalities detected during a DRE may signal the need for further investigations.Read more aboout DRE here.
If an abnormality is suspected, additional diagnostic tests may be recommended to confirm the presence of prostate cancer. These tests can include a prostate MRI scan, providing detailed imaging of the prostate gland, and a biopsy. During a biopsy, a thin needle is inserted into the prostate to collect tissue samples, which are then examined under a microscope. Read about MRI guided biopsy here.
The Gleason scoring system is a crucial component of assessing the biopsy results.
Pathological staging
The Gleason scoring system evaluates the microscopic appearance of prostate cancer cells to determine their level of differentiation from normal cells. It combines two numbers, with a higher score indicating a more aggressive and potentially faster-spreading cancer. Scores typically range from 6 (low risk) to 10 (high risk). This scoring system helps guide treatment decisions and predict the cancer's behaviour.See more here.
In recent years, the International Society of Urological Pathology (ISUP) has introduced a new grading system to enhance the precision of prostate cancer diagnosis. The ISUP scoring system provides a simplified five-grade classification, streamlining the interpretation of biopsy results and offering more accurate risk stratification for patients and their healthcare providers. This updated scoring system contributes to a more nuanced understanding of prostate cancer pathology, aiding in personalized treatment approaches and improved patient outcomes.
The International Society of Urological Pathology (ISUP) grading system classifies prostate cancer into distinct grades, each indicating the degree of aggressiveness and potential for spread. The ISUP system simplifies the traditional Gleason score into five categories, providing clearer guidance for treatment decisions based on the cancer's severity:
Grade Group 1 (Gleason Score 6):
Description: Low-grade cancer with well-differentiated cells.
Typical Treatment Options: Active surveillance (close monitoring), focal therapy, radical prostatectomy (surgical removal of the prostate), or radiation therapy.
Grade Group 2 (Gleason Score 3+4=7):
Description: Moderately differentiated cancer with a slightly higher risk of aggressiveness.
Typical Treatment Options: Treatment may include active surveillance, focal therapy, radical prostatectomy, or radiation therapy, depending on the patient's overall health and preferences.
Grade Group 3 (Gleason Score 4+3=7):
Description: Moderately aggressive cancer with more poorly differentiated cells.
Typical Treatment Options: Treatment options may lean towards more aggressive approaches, such as surgery or radiation therapy, depending on the specific characteristics of the cancer.
Grade Group 4 (Gleason Score 8):
Description: High-grade cancer with poorly differentiated cells, indicating an increased risk of progression.
Typical Treatment Options: Treatment often involves more aggressive interventions, such as surgery, radiation, or hormonal therapy.
Grade Group 5 (Gleason Score 9-10):
Description: Highly aggressive cancer with poorly differentiated cells and a higher risk of rapid spread.
Typical Treatment Options: Intensive treatments, including surgery, radiation therapy, and systemic therapies such as hormonal therapy or chemotherapy.
It is crucial to note that treatment decisions are individualized, considering various factors such as the patient's overall health, age, and preferences. Additionally, advancements in precision medicine and ongoing research contribute to the development of targeted therapies tailored to the specific characteristics of prostate cancer, further refining treatment options for optimal outcomes.
treatment strategies for localised prostate cancer
Active Surveillance:
Description: Monitoring low-risk prostate cancer with regular check-ups and tests.
Details: Suitable for Grade Group 1 and 2 cancers, avoiding immediate aggressive treatment.
Benefits: Minimizes overtreatment, preserving quality of life.
Considerations: Close monitoring to detect any progression.
Patient Profile: Older patients or those with limited life expectancy.
For a patient-friendly overview of active surveillance for prostate cancer, you can visit the Urology Institute information page here.
Focal Therapy:
Description: Targeted treatment focusing on specific cancerous areas.
Details: Uses techniques like Nanoknife – Focal Irreversible Electroporation (IRE) or high-intensity focused ultrasound (HIFU).
Benefits: Reduces side effects by sparing healthy tissue.
Considerations: Suitable for well-defined, localized tumours.
Patient Profile: Those seeking a balance between active treatment and preservation of function.
For a patient-friendly overview of fpcal therapy for prostate cancer, you can visit the Urology Institute information page here.
Radiotherapy:
Description: Using high-energy rays to kill cancer cells or inhibit their growth.
Details: External beam or brachytherapy (internal radiation) options.
Benefits: Non-invasive, effective in treating localized tumors.
Considerations: Potential side effects like urinary or sexual issues.
Patient Profile: Considered for patients who prefer non-surgical approaches.
Surgery (Robotic radical prostatectomy):
Description: Surgical removal of the prostate gland.
Details: Can be done traditionally or robotically (minimally invasive).
Benefits: Complete removal of cancer, potentially curative.
Considerations: Possible side effects like incontinence and erectile dysfunction.
Patient Profile: Generally younger, healthier individuals with localized cancer.
For a patient-friendly overview of surgery for prostate cancer, you can visit the Urology Institute information page here.
Treatment decisions for localized prostate cancer depend on factors such as cancer aggressiveness, patient preferences, and overall health. Discussing these options with healthcare providers is crucial to tailor a treatment plan that aligns with the patient's specific circumstances and goals.
Advanced prostate cancer
For a detailed patient-friendly overview of advanced prostate cancer, you can visit the Urology Institute information page here.
Advanced prostate cancer encompasses various stages and characteristics, reflecting the disease's progression beyond the initial confines of the prostate gland. Key terminologies include:
Metastatic Prostate Cancer:
Definition: Cancer that has spread beyond the prostate to distant sites, such as bones, lymph nodes, or other organs.
Characteristics: Presence of metastases indicates an advanced stage with a higher risk of complications.
Hormone-Naive Prostate Cancer:
Definition: Cancer that initially responds to androgen deprivation therapy (ADT) or hormonal treatment.
Characteristics: Typically at an earlier stage, with cancer cells sensitive to hormonal control.
Hormone-Resistant (or Castration-Resistant) Prostate Cancer:
Definition: Cancer that progresses despite initial hormone therapy.
Characteristics: Reflects the cancer's ability to adapt and continue growing despite lowered testosterone levels.
Non-Metastatic Castration-Resistant Prostate Cancer (nmCRPC):
Definition: Prostate cancer resistant to hormone therapy without evidence of distant metastasis.
Characteristics: Indicates a stage where the cancer is aggressive locally but has not yet spread to distant organs.
Locally Advanced Prostate Cancer:
Definition: Cancer that extends beyond the prostate but has not metastasized.
Characteristics: May involve nearby tissues or organs, posing challenges for complete surgical removal.
Understanding these terminologies is crucial for oncologists to tailor treatment strategies based on the specific characteristics of the cancer. Management of advanced prostate cancer often involves a combination of hormonal therapies, chemotherapy, targeted treatments, and radiation therapy to control disease progression, alleviate symptoms, and improve overall survival. Treatment decisions are individualized based on factors such as the patient's health, the extent of metastasis, and the responsiveness to hormonal interventions. For a detailed patient-friendly overview of advanced prostate cancer, you can visit the Urology Institute information page here.
treatment strategies for ADVANCED prostate cancer
Navigating the complexities of advanced prostate cancer requires a multifaceted approach, integrating cutting-edge medical therapies with a focus on holistic patient care. At the forefront of these treatment strategies are hormonal therapies, chemotherapy, and novel agents such as enzalutamide, apalutamide, and darolutamide, each playing a crucial role in managing the disease. This guide explores the evolving landscape of advanced prostate cancer treatments, emphasizing not only pharmaceutical interventions but also the growing recognition of the benefits derived from integrating exercise and physiotherapy into patient care. By addressing treatment’s medical and holistic aspects, we aim to provide insights into enhancing patient well-being and optimizing outcomes in the challenging journey of advanced prostate cancer.
Hormonal Therapy (Androgen Deprivation Therapy): Initial management involves suppressing testosterone to slow cancer growth, but resistance may develop over time.
Chemotherapy: For cases resistant to hormonal therapy, chemotherapy with drugs like docetaxel or cabazitaxel may target rapidly dividing cancer cells.
Anti-Androgen Therapies: Novel agents like enzalutamide, aniraterone, apalutamide, and darolutamide are increasingly used to block androgen receptors, hindering cancer progression and extending survival.
Exercise and Physiotherapy in Prostate Cancer Care: Incorporating exercise and physiotherapy into prostate cancer management is increasingly recognized for its valuable role. Physical activity not only contributes to overall well-being but may also help mitigate treatment side effects, improve cardiovascular health, and enhance quality of life. Physiotherapy, focusing on tailored exercises, may address issues such as incontinence or musculoskeletal challenges, aiding patients in maintaining functional independence and supporting their overall journey through advanced prostate cancer. Integrating these strategies into a comprehensive care plan can contribute to holistic patient well-being and treatment outcomes.
Additional diagrams, decision pathways, and patient-friendly resources are available on the Urology Institute website.