Vasectomy
What is involved in the vasectomy procedure?
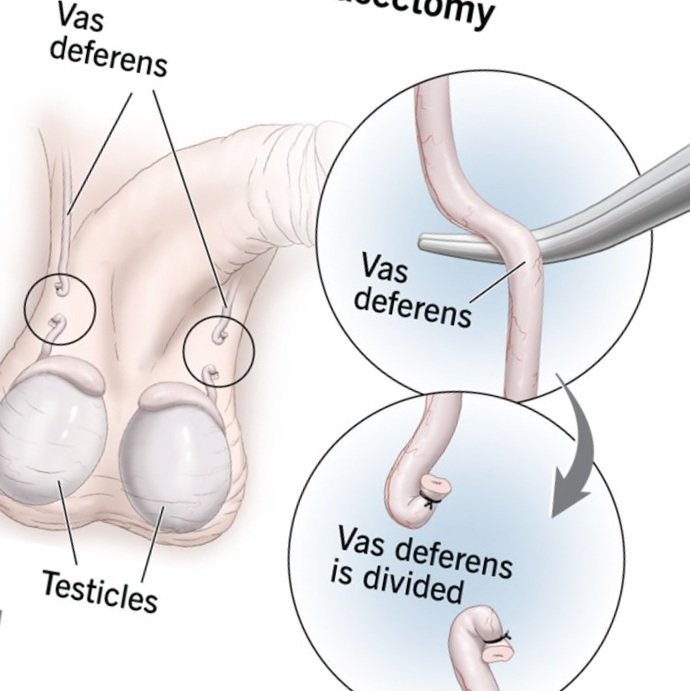
Vasectomy is a safe and effective permanent birth control method for men. During the procedure, the vas deferens, the tubes that carry sperm, are surgically cut or blocked to prevent sperm from reaching the semen. It is a minimally invasive outpatient procedure that takes less than 30 minutes. Vasectomy does not affect sexual function or libido, but it eliminates the risk of unintended pregnancy. It is a reliable and long-term solution for couples who have decided not to have more children. Recovery is usually quick, with most men able to resume normal activities within a few days.
Vasectomy can be done under local or general anaesthesia
Consider vasectomy as irreversible and avoid proceeding if uncertain. Typically, vasectomy isn't advisable during pregnancy or within the first six months postpartum, especially for men without children.
Vasectomy
main points
Key Points:
Vasectomy
Vasectomy is the most reliable form of male sterilization.
It is considered irreversible and should be approached as such.
Sterility is not immediate; alternative contraception is necessary until receiving clearance from post-operative semen tests, typically after 12 weeks and 20 ejaculations.
Late failure, resulting from the rejoining of vas deferens ends, occurs in approximately 1 in 2000 men.
Research has not found any evidence linking vasectomy to long-term health risks like testicular or prostate cancer.
Chronic testicular pain, affecting daily activities, may occur in up to 5% of cases but is generally manageable.
surgery
What occurs on the day of the procedure?
A/Prof Homi Zargar will discuss the surgery once again to ensure your understanding and obtain your consent.
Details of the procedure:
In cases where locating the tubes is challenging or if you have sensitivity to injections, a general anaesthetic is typically recommended.
Local anaesthesia may cause mild discomfort akin to a "bee sting" upon injection.
Two injections of local anaesthesia are administered, one on each side.
Once the anaesthesia takes effect, your skin will be numb, eliminating sharp or painful sensations while retaining the ability to feel touch, heat, and cold.
During the procedure, slight discomfort may occur when the surgeon manipulates each tube, potentially leading to temporary light-headedness, sweating, or nausea, which quickly diminishes.
Absorbable stitches are utilized to close the scrotal skin, disappearing within two to three weeks.
After-Effects and Risks of the Procedure:
Mild bruising and scrotal swelling accompanied by clear yellow fluid leakage from the wound after a few days: Nearly all patients experience this.
Presence of blood in semen during initial ejaculations: Occurs in between 1 in 2 to 1 in 10 patients.
Troublesome chronic testicular pain, impacting daily activities: Affects up to 1 in 20 patients.
Significant bruising and scrotal swelling necessitating surgical drainage: Seen in between 1 in 10 to 1 in 50 patients.
Epididymo-orchitis (testicular infection or inflammation): Occurs in approximately 1 in 10 to 1 in 50 patients.
Early failure indicated by persistent motile sperm in post-operative semen analysis, rendering the individual non-sterile: Seen in 1 in 250 patients.
Late failure due to the rejoining of vas deferens ends after initial negative sperm counts, leading to fertility and potential pregnancy: Affects 1 in 2000 patients.